- Key Takeaway: While high IgE levels don’t directly cause acne, there’s growing evidence suggesting complex interactions between allergic responses and acne development. High IgE is primarily associated with allergic conditions like eczema and atopic dermatitis, which can coexist with acne. Recent research shows mast cells in acne lesions express high-affinity IgE receptors, potentially contributing to inflammation, though the primary drivers of acne remain hormonal changes, bacterial colonization, and sebum production.
You know how frustrating it is when your skin breaks out and you’re trying to figure out what’s causing it. If you’ve had blood work done and noticed high IgE levels, you might wonder if there’s a connection to your acne. The relationship between IgE and acne isn’t as straightforward as you might think.
IgE antibodies are part of your immune system’s defense squad. They’re the ones that go into overdrive when you encounter allergens like pollen, dust mites, or certain foods. Normal IgE levels typically range from 1.5 to 150 kU/L, though this varies with age. When these levels spike above 200 kU/L, doctors start paying attention because it usually signals allergies, eczema, or parasitic infections.
Understanding the IgE-Acne Connection
Here’s where things get interesting. Acne vulgaris affects about 650 million people worldwide, and scientists have discovered that the immune system plays a bigger role than previously thought. The main troublemaker in acne is Cutibacterium acnes (formerly called Propionibacterium acnes), a bacteria that lives in your pores. But it’s not just about bacteria – it’s about how your immune system responds to them.
Recent studies have found that mast cells, which are immune cells loaded with IgE receptors, hang out in the upper dermis near blood vessels and nerve endings. These cells can trigger inflammatory responses when activated. In acne lesions, researchers have identified these high-affinity IgE receptors on mast cells, suggesting they might contribute to the inflammatory process. But here’s the catch – IgE isn’t the main culprit in acne development.
The primary drivers of acne are:
- Hormonal influences on sebum production (especially androgens).
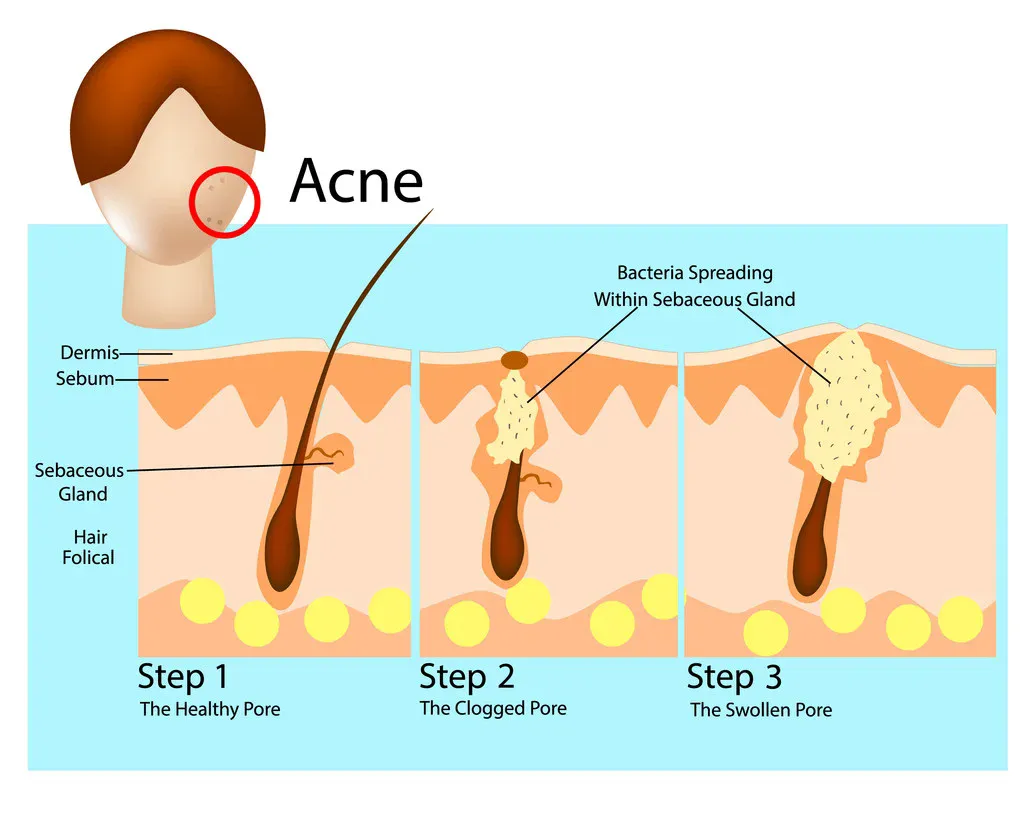
- Follicular hyperkeratinization (basically, dead skin cells clogging pores).
- Bacterial colonization by C. acnes.
- Inflammatory immune responses involving Th1 and Th17 lymphocytes.
When High IgE and Skin Problems Overlap
What’s more common is seeing high IgE levels alongside other skin conditions that can occur with acne. Atopic dermatitis, for instance, is characterized by elevated IgE levels, and studies show IgE concentrations tend to correlate with eczema severity. Some people have both eczema and acne, making their skin situation particularly complex.
Extremely high IgE levels (above 1000 kU/L) often indicate:
- Active atopic dermatitis or severe eczema.
- Chronic skin infections, including bacterial superinfections.
- Hyper-IgE syndromes (rare genetic conditions).
- Parasitic infections.
- Certain immune deficiency disorders.
Research has shown that children with atopic dermatitis and IgE levels above 1001 IU/mL were 66 times more likely to develop skin superinfections compared to those with levels below 300 IU/mL. These superinfections, particularly with Staphylococcus aureus, can sometimes be mistaken for or complicate acne.
The Inflammatory Loop in Your Skin
Your skin has what scientists call an epithelial-immune microenvironment (EIME). This includes your skin barrier, immune cells, nerve endings, and the bacteria living on your skin. When this system gets disrupted, inflammatory loops can develop. In acne, multiple inflammatory pathways get activated:
The innate immune system recognizes C. acnes through toll-like receptors (TLRs), triggering inflammation. This leads to the production of inflammatory cytokines, matrix metalloproteinases (MMPs), and antimicrobial peptides. The adaptive immune response kicks in too, with Th17 and Th1 cells playing major roles in early acne development.
Interestingly, while IgE-bearing mast cells are present in acne lesions, the inflammatory response in acne is primarily driven by other immune pathways. The role of IgE in acne appears to be more of a supporting actor rather than the lead character.
What This Means for Your Skin
If you have high IgE levels and acne, several scenarios might be at play:
You might have overlapping conditions. High IgE could indicate allergies or eczema occurring alongside acne. Each condition needs separate attention, though some treatments might help both.
Food sensitivities could be involved. While the diet-acne connection remains controversial, some research suggests high-glycemic foods and dairy might worsen acne in certain individuals. If you have food allergies (indicated by high specific IgE), avoiding trigger foods might improve overall skin health.
Your immune system might be overreactive. Some people have generally heightened immune responses, leading to both allergic conditions and more severe inflammatory acne.
Testing and Treatment Considerations
If you’re dealing with both high IgE and acne, here’s what might help:
- Get specific IgE testing. Total IgE tells you there’s inflammation or allergy somewhere, but specific IgE tests can identify particular triggers. This is especially useful if you suspect food allergies or environmental allergens are affecting your skin.
- Address both conditions. Treating underlying allergies or eczema might reduce overall skin inflammation, potentially helping acne too. But you’ll still need acne-specific treatments.
- Consider your skincare routine. If you have sensitive, allergy-prone skin, harsh acne treatments might cause more problems. Look for gentler alternatives and patch-test new products.
- Work with specialists. A dermatologist can help with acne management, while an allergist can address high IgE levels and potential allergies. Sometimes you need both perspectives.
The Bottom Line
High IgE levels don’t directly cause acne, but they indicate an overactive immune response that might complicate your skin situation. The immune cells bearing IgE receptors do show up in acne lesions and might contribute to inflammation, but they’re not the primary drivers.
If you have elevated IgE along with acne, you’re likely dealing with multiple issues that need addressing. Focus on identifying and managing any allergic conditions while treating your acne appropriately. Remember that acne is primarily driven by hormones, bacteria, and specific inflammatory pathways – not by IgE-mediated allergic responses.
The good news? Understanding these connections helps you take a more comprehensive approach to skin health. Instead of looking for a single cause, you can work with healthcare providers to address all the factors affecting your skin.
References